Surgery for Syndromes
Surgical Procedures for Craniofacial Syndromes
Children with conditions affecting the head and face often need surgery to give their brain room to grow. Many children need bones in their face moved and enlarged to improve their breathing, chewing and appearance.
For many procedures, we recommend surgery to cut bones followed by distraction osteogenesis to slowly lengthen the bones. The combination lets us move and enlarge bones more than traditional surgery alone. Our team works together and with you to decide what is right for your child.
Our team is experienced in the techniques children with complex craniofacial conditions may need:
- Posterior cranial vault distraction to give the brain room to grow
- Fronto-orbital advancement to enlarge the skull and protect the eyes
- Le Fort III midface advancement to move the middle of the face forward
- Monobloc frontofacial advancement to reposition the forehead and midface
- Segmental subcranial distraction to normalize the proportions of the face
- Counterclockwise craniofacial distraction osteogenesis (C3DO) to improve the airway and jaw position
- Le Fort I maxillary advancement to help the teeth and jaws fit together
- Mandibular osteotomy with distraction or internal fixation to correct a lower jaw
Posterior Cranial Vault Distraction
Posterior cranial vault distraction expands the back of the skull to give the brain room to grow. This is mainly used if your child needs more space than can be provided by surgery on the front of their skull alone.
Your child may need this if they have Apert, Crouzon or Pfeiffer syndrome. It can also help if your child has multiple suture synostosis that is not part of a syndrome, such as cloverleaf skull deformity.
Most often, this surgery is done at about 6 months of age. It creates enough space to prevent pressure on your baby’s brain. This allows surgery on the front of their skull to be done after 1 year of age. If frontal surgery is done before 1 year, there is a higher risk that the surgery will have to be repeated.
-
How posterior cranial vault distraction works
- The operation takes 3 hours.
- A plastic surgeon and neurosurgeon work together in the operating room.
- The surgeons make a cut around the back of your child’s skull bone and attach distractors across the cut. Distractors are small metal devices that help expand the skull by slowly stretching 2 pieces of bone apart. Learn more about distraction osteogenesis.
- The distractors are placed under the skin. They have posts that pass through the skin to allow adjustment.
- Most children stay in the hospital 3 days. The first night they are closely monitored in the intensive care unit (ICU).
- While your child is recovering at home over the next 2 to 3 weeks, a parent or other caregiver turns a screw to adjust each distractor. This increases the gap in the back of your child’s skull 1 to 2 millimeters a day.
- New bone grows to fill in the gap. After 2 to 3 months, the new bone heals and the back of the head is larger.
- The distractors are removed in a short operation after the new bone has healed.
Some children need to have this surgery again when they are 2 to 5 years old. That may happen if a child’s skull grows abnormally or does not expand enough to fit their growing brain.
Fronto-Orbital Advancement
Fronto-orbital advancement helps protect the eyes and makes the skull bigger so the brain can grow.
This surgery is needed by most children with craniosynostosis that is caused by a syndrome. These syndromes include Apert, Crouzon, Saethre-Chotzen, Muenke and Pfeiffer.
The timing of front-orbital advancement depends on your child:
- It is done during the first year of life if needed to protect your child’s eyes.
- Most children with syndromic craniosynostosis have this surgery between 1 and 2 years of age.
- Children with most types of nonsyndromic craniosynostosis have fronto-orbital advancement when they are 9 to 12 months old.
- Less often, children with craniosynostosis of the sagittal suture need this surgery to reshape the front of their skull at 2 years or later.
-
How fronto-orbital advancement works
- Surgery usually takes 5 hours.
- A plastic surgeon and neurosurgeon work together during the operation.
- They move the forehead and the upper eye sockets forward. They reshape the forehead to make it wider.
- The plastic surgeon takes a bone graft from your child’s hip or ribs and uses it to support the bones in their new position.
- Small metal plates or screws hold the bone in its new shape until it heals. These are absorbed by the body over time.
- Most children stay in the hospital 4 days. The first night they are closely monitored in the ICU.
- This procedure does not involve distraction osteogenesis.
Le Fort III Midface Advancement
Le Fort III midface advancement brings the entire upper jaw and the cheekbones forward. Le Fort III refers to the entire midface, which moves as 1 piece of bone. The operation is also called Le Fort III osteotomy.
The surgery helps children breathe and chew better. It protects their eyes and improves how their face looks.
Our team, led by our surgical director, Dr. Richard Hopper, performs more of these surgeries each year than most other centers in the country.
Midface advancements can be done by:
- Surgery alone using metal plates and screws and bone grafts from other parts of the body
- Surgery followed by distraction osteogenesis to slowly stretch 2 pieces of bone apart and create a longer one
For many children, surgery with distraction is a better choice. It lets us move the bone farther to account for later growth. This can reduce how much surgery your child needs as they grow. With distraction, there is no need for bone grafts from other parts of the body. No metal plates are left behind.
-
Timing of Le Fort III
- Midface distraction is often done when children are 8 to 10 years old.
- If breathing is a problem, your doctor may recommend doing it as young as 3 years old.
- The older a child is, the less growing they have left to do, and the less likely they will need another major procedure for the midface.

BEFORE (Above, left): The middle of this girl's face did not grow well because of Crouzon syndrome. This caused severe breathing problems.
DISTRACTION (Above, center): The distractor is attached during surgery that separates the face bones. The device is used for about 2 months.
AFTER (Above, right): As a result, the child has a larger airway so she can breathe better during sleep. Her cheekbones are larger and her teeth fit together better.
Her upper jaw is finished growing, but her lower jaw will keep growing for several years. When her bones have finished growing (about age 16), her jaws will be a good fit.
-
How midface advancement with distraction works
- This is a full-day operation.
- During the operation, surgeons separate the bones of your child’s face from their skull so that all the facial bones can be moved.
- The surgeons attach the distractor to your child’s skull and the central part of their face, which is still mobile.
- How many days your child will be in the hospital depends on their condition. For the first few days they will be closely monitored in the ICU.
- While your child is recovering at home, a parent or other caregiver turns little screws to adjust the distractor every day for 2 to 3 weeks. This brings the upper jaw and cheekbones forward (away from the skull). New bone grows and fills in the gaps.
- Once everything is in the right place, the distractor stays on for up to 8 more weeks. This helps the bone heal in its new position.
- After healing, the distractor is removed in a short operation. Your child goes home the same day as the surgery.

SMALL SCAR: At Seattle Children's, our Le Fort III method helps prevent scars on your child's face. It leaves a single scar hidden in the hair. To connect the upper jaw to the device, we use small incisions and a custom splint that fits in your child's mouth. We do not cut the mouth or the eyelids or place posts in their cheeks, as most other hospitals do.
Monobloc Frontofacial Advancement
Monobloc frontofacial advancement surgery moves the bones of the forehead and middle of the face (midface) forward. Surgeons also open the closed joints (sutures) at the front of your child’s skull.
The surgery gives more space for your child’s growing brain. It helps with breathing, eye protection, chewing and appearance. A child may need this procedure if they have a genetic condition that makes the fibrous seams in the skull (sutures) close early, such as Saethre-Chotzen syndrome.
The monobloc procedure is usually done when a child is 8 to 12 years old. But some children need this surgery before they are 2 years old.
Depending on how your child grows, they may need other surgery to adjust the forehead or midface as they get older.
-
How monobloc frontofacial advancement works
This surgery combines fronto-orbital advancement and Le Fort III midface advancement procedures.
- The operation takes 6 to 8 hours.
- A plastic surgeon and neurosurgeon work together during the operation.
- After surgery, most children stay in the hospital 5 to 7 days. The first 3 days they are closely monitored in the ICU.
- Most often, the surgery is followed by distraction osteogenesis to grow a longer bone using a device called a distractor. While your child heals at home, a parent or other caregiver adjusts the distractor each day. This pulls the pieces of the cut bone apart slowly over several weeks. New bone grows to fill in the gaps.
- If distraction is not used, the bones are moved forward during surgery and fixed in place with bone grafts, screws and plates.
Segmental Subcranial Distraction
For children with Pfeiffer syndrome and Apert syndrome, our team developed segmental subcranial distraction to treat their symptoms and appearance better than the traditional approach (Le Fort III advancement).
Segmental subcranial distraction makes the proportions of the face more normal in children with these 2 conditions. As a result:
- Your child’s nose is longer
- There is a protective curve to their face
- Their eyes are more level and are protected by surrounding bone
- Your child can breathe and chew more easily
Our patients like the change in how their face looks.
-
Benefits compared to traditional treatment
The traditional treatment for Apert and Pfeiffer syndromes (Le Fort III advancement) helps children breathe and chew better. But segmental subcranial distraction does more to improve a child’s appearance when viewed from both the front and the side.
Le Fort III brings several bones in the midface forward the same distance and in 1 direction. Our team uses segmental subcranial distraction to move the cheekbones, upper jaw and forehead different amounts and in different directions.
An analysis of patients’ computed tomography (CT) scans showed that segmental subcranial distraction is more effective in normalizing facial proportions than the Le Fort III procedure. It results in better appearance, chewing and breathing, compared to Le Fort III. The study results were published in the journal of the American Society of Plastic Surgeons.
We are currently doing research on how the procedures compare over the long term as a child becomes an adult.


BEFORE (Left): The middle of this boy's face did not grow well because of Apert syndrome. His forehead is high and flat. His cheekbones are sunken. His jaws do not fit together well.
AFTER (Right): As a result of segmental subcranial distraction, the boy's cheekbones have been moved forward and upward. His nose, upper jaw and teeth have moved forward and down a greater distance. His forehead has been smoothed. His face looks more typical. His teeth fit together better.
His upper jaw is finished growing, but his lower jaw will continue to grow. To anticipate future growth, surgeons overcorrect the position of the jaw and midface. This reduces the extent of any jaw-balancing surgery at adulthood.
-
How segmental subcranial distraction works
This procedure combines surgery and distraction osteogenesis, a way to grow a longer bone by slowly stretching 2 pieces of bone apart.
- The delicate surgery takes 6 hours.
- In the operating room, surgeons separate the bones of your child’s face from their skull so that the entire face is mobile.
- Their cheekbones and outer eye sockets are then released from the middle of their face.
- Surgeons move the cheekbones into a more normal position
- Small titanium plates hold the cheekbones in their new place. In this position, the cheekbones now support the eyes.
- If the forehead needs to be smoothed out, surgeons may apply a custom implant designed specifically for your child.
- Surgeons attach the distractor to the central part of your child’s face, which is still mobile. They use a splint on your child’s teeth, with wires that attach to the bone under the skin. This avoids scarring. The distractor helps to stabilize the mobile bones.
- The upper jaw is not advanced during the surgery. Movement of the upper jaw takes place slowly as the distractor is turned.
- After surgery, most children spend 7 days in the hospital. The first 3 nights are in the ICU. They are sedated and have a breathing tube until swelling in the airway goes down.
Adjusting the distractor to grow new bone
- As your child recovers at home for 2 to 3 weeks, a parent or other caregiver turns a screw on the distractor every day. This moves the upper jaw forward and down. New tissue grows to fill in the gaps.
- The amount and direction of movement is customized to your child.
- Once everything is in the right position, the distractor stays on for about 6 weeks to help the bone heal in its new position.
- After healing, the distractor is removed during a short surgery. Since the distractor is on the outside of the face, no cuts or stitches are needed. Your child does not need to spend the night in the hospital.
Counterclockwise Craniofacial Distraction Osteogenesis (C3DO)
We recommend counterclockwise craniofacial distraction osteogenesis (C3DO) for children with Treacher Collins syndrome who have had a breathing tube inserted into their windpipe (tracheostomy). Usually, C3DO is done when your child is 6 to 10 years old.
Seattle Children’s Craniofacial Center is the first to use C3DO to improve the airway and jaw position in children with Treacher Collins syndrome. The goal is to enable your child to breathe without a tube in their windpipe. Surgeons around the world are adopting our approach.
C3DO gets better results than the traditional treatment because it combines 2 separate procedures: mandible distraction and Le Fort II nasomaxillary advancement. Performing 2 procedures at the same time makes a bigger correction in the backwards jaw rotation caused by Treacher Collins syndrome. The combined surgery helps open your child’s airway.
- Read how Nathaniel found freedom after surgery that lets him breathe without a tracheostomy for the first time.
- Read more about C3DO in Plastic and Reconstructive Surgery: Journal of the American Society of Plastic Surgeons.
-
How counterclockwise craniofacial distraction osteogenesis works
This procedure combines surgery and distraction osteogenesis, a way to grow a longer bone by slowly stretching 2 pieces of bone apart.
- The surgery is a full-day operation.
- Surgeons separate both jaws from the skull (complete subcranial facial separation). This makes the entire face mobile.
- The surgeons attach a U-shaped headframe to your child’s skull using a series of pins. They use wires to fasten the distractor to a splint that is fitted on your child’s upper teeth.
- Next, the surgeons attach a second metal distractor to your child’s lower jaw using pins through the skin. They wire your child’s jaws together.
- If your child does not already have one, doctors will place a tube through your child’s nose and into their stomach. The tube is removed as soon as your child can eat liquid food through their mouth. This is similar to someone with a broken jaw that is wired during healing.
- After surgery, most children stay in the hospital 5 or 6 days. The first 3 days they are closely monitored in the ICU.
Adjusting the distractor at home
- While your child is at home, a parent or other caregiver turns little screws to adjust the distractors every day for 2 to 3 weeks. This makes the entire face move forward slowly, rotating from the point where the nose meets the forehead. New bone grows and fills in the gaps.
- This movement corrects the backwards rotation of the jaw and opens the narrowed airway.
- After the distractor adjustment period is finished, your child’s doctor removes the wires holding the jaws shut. This lets your child open and close their mouth. For the rest of the healing process, your child can eat a soft, no-chew diet. See tips on a no-chew diet (PDF).
- Once everything is in the right place, the distractors stay on for 8 to 12 weeks. This helps the bones heal in their new position.
- After healing, a surgeon removes the distractors in a short operation. Your child goes home the same day as the surgery.
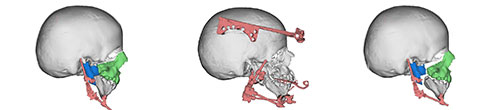
LEFT: The blue and green areas of the image show where surgeons separated the upper and lower jaws from the skull. The distractor device on the lower jaw is shown in pink.
MIDDLE: This procedure uses 2 distractor devices: a headframe on the skull and a mandible device on the lower jaw.
RIGHT: After surgery, turning screws on the distractors moves the entire face forward, away from the skull. New bone grows to fill in the gaps between the eye sockets and green area and between the lower jaw and blue area. As a result, the jaw rotates and moves forward. This opens the airway.
Le Fort I Upper Jaw Advancement
In some children, their upper jaw (maxilla) does not grow as well as the rest of their face. When they close their jaws, the upper teeth are behind the lower teeth.
This happens with many craniofacial conditions, including cleft palate, syndromic craniosynostosis and Treacher Collins syndrome.
We recommend Le Fort I maxillary advancement surgery to improve how your child’s jaws and teeth fit together. It can also improve breathing through the nose.
Most often this surgery is done after your child’s bones have finished growing. This happens at 16 years of age for most girls and at 18 years of age for most boys.
If the upper jaw needs to move forward a large distance, the surgery takes place sooner. By age 12, a child usually has enough adult teeth to make the surgery possible.
-
How Le Fort I surgery works
Our plastic surgeon works closely with our craniofacial orthodontist to plan and carry out your child’s treatment. Your child’s orthodontist will use braces or appliances to put the teeth in the best position before surgery.
The operation takes 3 to 4 hours. Most children stay in the hospital 2 to 3 days.
During the operation, the surgeon makes cuts under the upper lip and then cuts the upper jaw on both sides of the face.
Once the upper jaw is mobile, the surgeon will move part of the jawbone forward.
Moving the upper jaw without distraction
- If the upper jaw needs to be moved less than half an inch, the bone is moved into its new position during the surgery.
- The surgeon uses metal plates and screws to hold it in the new position.
- The plates and screws do not usually need to be removed.
Moving the upper jaw with a distractor
- If the upper jaw needs to be moved half an inch or more, your child’s surgeon will use a metal device called a distractor. It lengthens a bone by slowly stretching 2 pieces of bone apart. Learn more about distraction osteogenesis.
- After cutting the jaw, the surgeon attaches an external distractor to your child’s skull with a series of pins. The doctor uses wires to attach the distractor to a splint that is fitted on your child’s upper teeth.
- While your child recovers at home, a parent or other caregiver adjusts the distractor to slowly move the bone. The parent turns a screw on the distractor 1 to 2 millimeters a day.
- In about 2 weeks the upper teeth and the surrounding bone have moved forward to the correct position.
- For 6 to 8 more weeks, the distractor holds the jaw in place until the bone heals in this new position.
- The distractor is removed during a short surgery. Your child does not have to spend the night in the hospital.
Mandibular Osteotomy With Distraction or Internal Fixation
If the lower jaw (mandible) does not grow properly, your child may have problems with breathing because their tongue is pushed to the back of their throat. The lower teeth bite far behind the upper teeth, making it hard to chew. When the teeth fit together poorly, it is called malocclusion.
A number of conditions may cause this. Among them are craniofacial (hemifacial) microsomia, Treacher Collins syndrome, Pierre Robin sequence and craniosynostosis syndromes, including Apert, Crouzon, Saethre-Chotzen, Muenke and Pfeiffer.
The procedure that is right for your child depends on their age and health needs. The options include:
- Fixing the lower jaw in place with plates and screws during surgery (mandibular osteotomy with internal fixation).
- Double jaw surgery. If both the upper and lower jaws need to be corrected, mandibular osteotomy can be combined with a Le Fort I osteotomy.
- Using a distractor device to enlarge the lower jaw after surgery (mandible distraction).
-
Mandibular osteotomy with internal fixation
If a child has finished growing and needs their lower jaw moved to fit their upper jaw, we perform mandibular osteotomy with internal fixation. This is the most common way to change the position of a jaw.
- The surgeon cuts your child’s lower jaw and moves it either forward or backward.
- The surgeon fixes the jaw in its new position with small metal plates and screws (internal fixation).
- Rarely, a bone graft from another part of the body is needed. If needed, the surgeon may use bone from one of your child’s jaws or from their upper hip.
- This surgery is done when a child’s bones have finished growing. For most girls, that happens by 16 years of age. For most boys, by age 18.
- There are several variations of this procedure.
-
Mandible distraction
If larger movement in jaw position is needed or the jaw must be moved before a child has finished growing, we recommend mandible distraction.
Read Lexi’s story: Doctors Create a Jaw for Little Girl Born Without One.

Left: This young girl’s jaw did not form properly as a result of auriculo-condylar syndrome. Surgeons will cut her lower jaw so it can be moved forward and made longer.
Middle: After surgery, her parents adjust the distractor each day to slowly lengthen and advance her jaw.
Right: As a result, the girl has a larger lower jaw that makes it easier to breathe.
- Mandible distraction starts with surgery to make a cut on both sides of the lower jaw. After surgery, distraction osteogenesis enlarges the lower jaw.
- The surgeon places a small metal distractor across the gap in the cut bone. Most often, the distraction device fits under the skin. It has a small post that passes through the skin for adjusting the distractor.
- In rare cases, when a very large movement of the lower jaw is needed, the surgeon uses a larger distraction device that fits outside the skin. It attaches to the jaw with pins through the skin.
- The operation takes 2 to 4 hours. The hospital stay varies from 2 days to 2 weeks or longer, depending on your child. Some children may need to be monitored in the ICU part of that time.
- After your child goes home, a parent or other caregiver turns a screw to adjust the device. Over a couple of weeks, this slowly moves the lower jaw forward and makes it longer.
- Once the jaw has moved forward enough, the distractor holds the new position while the jaw heals. This takes 8 to 12 weeks. The device is removed during a small second surgery. If your child’s distractor is under their skin, they will spend a night in the hospital. No hospital stay is needed if your child has an external distractor.
See how distraction osteogenesis was used for a child born with bilateral craniofacial microsomia:
 The young child in this example was born with bilateral hemifacial microsomia, with his right side more affected than the left.
The young child in this example was born with bilateral hemifacial microsomia, with his right side more affected than the left. A break (osteotomy) is made on both sides of the jaw and a mechanical device called an external distractor is placed during an operation.
A break (osteotomy) is made on both sides of the jaw and a mechanical device called an external distractor is placed during an operation. As the distractor is slowly opened at one millimeter a day during the month after the surgery, the gaps in the bone increase in size. After the new lower jaw has been enlarged to the correct size, new bone forms spontaneously in the gaps.
As the distractor is slowly opened at one millimeter a day during the month after the surgery, the gaps in the bone increase in size. After the new lower jaw has been enlarged to the correct size, new bone forms spontaneously in the gaps. The child now has a larger and symmetric jaw made of bone that his body grew by itself. This larger jaw will help breathing and chewing.
The child now has a larger and symmetric jaw made of bone that his body grew by itself. This larger jaw will help breathing and chewing.Improving Outcomes at Each Step
Our goal is to minimize the number of steps in your child’s treatment plan by improving the outcome of each step. Our work to refine surgery for children with Apert syndrome and Treacher Collins syndrome is changing the practice of surgeons around the country.
Our team includes pediatric craniofacial plastic surgeons, neurosurgeons, oral and maxillofacial surgeons and surgical craniofacial orthodontists. During surgery affecting the skull, a neurosurgeon and craniofacial plastic surgeon work as a teamin the operating room.
To help plan your child’s treatment and surgery, we use 3-D imaging and advanced software to build precise maps of your child’s face and skull. 3-D imaging technology allows our doctors to predict how movement in one part of the face is likely to affect other areas. It also accounts for future growth.
This helps the surgeon and orthodontist plan exactly how much to move different bones of the face and in which direction. We plan for the desired position of bones at adulthood.
Advance planning also shortens the surgery and the time your child is under anesthesia.
Improving Outcomes at Each Step
Our goal is to minimize the number of steps in your child’s treatment plan by improving the outcome of each step. Our work to refine surgery for children with Apert syndrome and Treacher Collins syndrome is changing the practice of surgeons around the country.
Our team includes pediatric craniofacial plastic surgeons, neurosurgeons, oral and maxillofacial surgeons and surgical craniofacial orthodontists. During surgery affecting the skull, a neurosurgeon and craniofacial plastic surgeon work as a team in the operating room.
To help plan your child’s treatment and surgery, we use 3-D imaging and advanced software to build precise maps of your child’s face and skull. 3-D imaging technology allows our doctors to predict how movement in one part of the face is likely to affect other areas. It also accounts for future growth.
This helps the surgeon and orthodontist plan exactly how much to move different bones of the face and in which direction. We plan for the desired position of bones at adulthood.
Advance planning also shortens the surgery and the time your child is under anesthesia.