Kidney Transplant Surgery
Getting the Go-Ahead
Deceased-donor kidney transplants
When a kidney from a deceased donor is available, an organ procurement organization contacts Seattle Children’s.
Both a transplant nurse coordinator and a transplant surgeon are on call 24 hours a day at Seattle Children’s. The transplant nurse coordinator and the transplant surgeon will discuss the history and condition of the donor to determine if this donor organ would be a good match for your child.
If the organ is a good match, the transplant nurse coordinator will contact you to see if your child is able to undergo the transplantation surgery. The coordinator must make sure that your child does not have any new health problems that require delaying transplantation, such as a cold or the flu.
United Network for Organ Sharing (UNOS) policy requires that the transplant center (your Seattle Children’s transplant team) decides whether or not to accept the kidney offer within 1 HOUR.
Living-donor kidney transplants
If you and the transplant team have decided on a living-donor transplant and a donor has volunteered and been approved, Seattle Children’s and University of Washington Medical Center (UWMC) will coordinate your child’s surgery with the surgery of the person donating their kidney. The surgeries will happen the same day at about the same time.
Preparing for Surgery
If the kidney is coming from a deceased donor, we will do a crossmatch test to make sure that your child doesn’t already have an immune response (antibodies) to the donor kidney. The crossmatch is done by mixing your child’s blood with cells from the donor.
- If the crossmatch is positive, it means that your child has an immune response against the donor kidney and should not receive this particular organ because the kidney will be rejected.
- lf the crossmatch is negative, it means your child does not have an immune response to the donor kidney and is eligible to receive this organ.
If your child is receiving a kidney from a living donor, we will do the final crossmatch at a clinic visit a few days before the date of the scheduled transplant surgery.
We will not begin medicines to suppress the immune system until your child’s crossmatch with the donor kidney is known to be negative.
If your child is receiving a kidney from a deceased donor, the time of surgery is planned for about the same time that the donated kidney arrives at our hospital. The kidney cannot live long outside a body, so it must be removed from the donor, transported quickly to Seattle Children’s and then transplanted into your child within a few hours.
Kidney Transplant Surgery
A kidney transplant involves placing the donor kidney into your child’s abdomen just above the pelvis. In the normal position, kidneys are located high in the back of the abdomen and well protected by the ribs, behind other organs such as the liver and stomach.
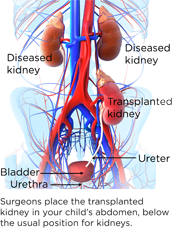 When the kidney is removed from the donor, important blood vessels (the renal artery and renal vein) that bring blood to and from the kidney, as well as the ureter, are taken out with it. During the transplant surgery, these blood vessels are attached to an artery and vein in your child to re-establish blood circulation to the kidney. The ureter, which is the tube that drains urine from the kidney to the bladder, is reattached to your child’s bladder to allow the urine to drain in the normal manner.
When the kidney is removed from the donor, important blood vessels (the renal artery and renal vein) that bring blood to and from the kidney, as well as the ureter, are taken out with it. During the transplant surgery, these blood vessels are attached to an artery and vein in your child to re-establish blood circulation to the kidney. The ureter, which is the tube that drains urine from the kidney to the bladder, is reattached to your child’s bladder to allow the urine to drain in the normal manner.
Removal of diseased kidneys
In certain situations, doctors may recommend taking out your child’s diseased kidneys before the transplant surgery or at the time of the kidney transplant.
If your child has problems with kidney or urine infections or loses too much protein or water from the diseased kidneys before transplant, these problems may continue after transplant and interfere with the function of the newly transplanted kidney.
Also, if the diseased kidneys are too large to leave room for the transplant, or if your child has extremely high blood pressure despite the best medical management, kidney removal (nephrectomy) may be recommended.
Stent placement
A stent may be placed in your child’s ureter during the transplant surgery. A stent is an internal tube to help protect the ureter–bladder connection as it heals and to make sure urine flows easily from the kidney into the bladder.
The stent will need to be removed several weeks after the transplant. This procedure involves using a small scope to look into the bladder and remove the stent from the ureter. Stent removal is usually done as an outpatient surgical procedure during the day.
Updates and communication with you
The operating room staff will let you know how your child is doing during the surgery. They will contact you through the pager you picked up from the NICU.