Hydrocephalus
-
Schedule an appointment with the Neurosciences Center
If this is a medical emergency, call 911.
- If you would like an appointment, ask your child’s primary care provider for a referral.
- If you have a referral, call 206-987-2016 or 844-935-3467 (toll-free).
- How to schedule.
If you have any questions, please contact us at 206-987-2016 or 844-935-3467 (toll-free).
-
Find a doctor
- Meet the Neurosciences team.
-
Locations
- Seattle Children’s hospital campus: 206-987-2016 or 844-935-3467 (toll-free)
- Bellevue Clinic and Surgery Center: 206-987-2016 or 844-935-3467 (toll-free)
- Everett: 425-783-6200
- Federal Way: 206-987-2016 or 844-935-3467 (toll-free)
- Olympia: 206-987-2016 or 844-935-3467 (toll-free)
- Tri-Cities: 206-987-2016 or 844-935-3467 (toll-free)
- Wenatchee: 206-987-2016 or 844-935-3467 (toll-free)
-
Refer a patient
- Urgent consultations (providers only): call 206-987-7777 or 877-985-4637 (toll free).
- If you are a provider, fax a New Appointment Request Form (NARF) (PDF) (DOC) to 206-985-3121 or 866-985-3121 (toll-free).
- Send the NARF, chart notes and any relevant documentation to 206-985-3121 or 866-985-3121 (toll-free).
What is hydrocephalus?
An MRI scan of a brain with hydrocephalus (left) and a normal MRI scan (right). The large dark area on the left is the ventricles, made bigger by a build-up of CSF.
Hydrocephalus (pronounced hi-dro-SEF-a-lus) is a harmful buildup of cerebrospinal fluid (CSF) in the ventricles of your child’s brain. CSF is a clear fluid that bathes and protects your child’s brain and spinal cord. Ventricles are the spaces in the brain where CSF is made.
The word “hydrocephalus” means water (hydro) in the head (cephalus). This problem is sometimes called water on the brain. The “water” is actually CSF.
Normally, CSF flows from the ventricles through the brain and into the space around the brain and spinal cord. A child’s body is always making and absorbing CSF.
When CSF cannot flow or does not get absorbed the way it should, fluid builds up. This is hydrocephalus. The buildup puts pressure on your child’s brain. Without treatment, hydrocephalus can cause problems with how your child’s brain develops and how it works. Pressure on the brain from hydrocephalus can be deadly.
-
Causes of hydrocephalus
CSF may not be able to flow as it should because of the way your child’s brain formed. This is called congenital hydrocephalus.
Hydrocephalus that happens for any other reason is called acquired hydrocephalus. Causes include:
- Bleeding inside the ventricles of the brain (intraventricular hemorrhage)
- Head injury
- Brain infection
- Brain tumor
Hydrocephalus at Seattle Children’s
All Seattle Children’s neurosurgeons are experts in treating this condition. We perform more than 200 hydrocephalus surgeries a year. We are also international leaders in hydrocephalus research.
See our Neurosciences statistics and outcomes.
If you would like an appointment, ask your child’s primary care provider for a referral. If you have a referral, call 206-987-2016 to make an appointment.
If you have questions, please contact our Neurosciences Center at 206-987-2016.
-
The experts you need are here
- Dr. Samuel R. Browd is known internationally for treating children with hydrocephalus and leading research to improve their care.
- In our Neurodevelopmental Clinic, experts in many medical areas work together to care for children if hydrocephalus causes problems in their thinking, balance, learning or emotions. We work with children long-term to help them reach their full potential.
- If your newborn is critically ill due to hydrocephalus, we provide specialized care in our Neuro NICU – the only neonatal neurocritical care program in Washington, Wyoming, Alaska, Montana and Idaho.
-
The most advanced treatments
- Most children with hydrocephalus need surgery to place a tube (shunt) in their brain to drain extra fluid. We make 3-D models of your child’s brain before surgery and operate with “GPS-guidance” to place shunts with precision. This has dramatically reduced the need for shunt revisions in children we treat.
- At Seattle Children’s, we have one of the lowest shunt infection rates in the nation (3% compared to the national average of 15%). To reduce the risk of infections, we use a standard process for doing shunt surgery and giving antibiotics.
- For some babies, we offer treatment options that avoid the need for a shunt. In endoscopic third ventriculostomy (ETV), neurosurgeons create a pathway so CSF can flow to areas of the brain where it is absorbed. Surgeons then heat the part of the brain that makes CSF, so less fluid is produced. This procedure is called choroid plexus cauterization (CPC). Your doctor will offer this option if it’s a good choice for your child.
- Because children who have hydrocephalus need many imaging scans of their heads during childhood, we use rapid-sequence MRI to avoid exposing them to radiation. If CT (computed tomography) scans are needed, we use lose-dose CT scans to reduce the amount of radiation children get (only ¼ to ½ of the usual dose).
-
Research to improve care
- We aim to cut shunt failure rates in half. Seattle Children’s is a national leader in research to improve shunts.
- Dr. Ghayda Mirzaa does basic science research to understand the genetic basis for hydrocephalus. Our goal is new ways to treat hydrocephalus.
- Seattle Children’s is part of a group of leading children’s hospitals that work together on research studies (clinical trials) to improve hydrocephalus care for all children. The group is called the Hydrocephalus Clinical Research Network (HCRN). Together, we keep a registry of children with hydrocephalus that helps us better understand the condition and develop new treatments. Dr. Jay Hauptman leads this research at Seattle Children’s.
- Seattle Children’s team has trained neurosurgeons from around the world in hydrocephalus treatment. These neurosurgeons return to their home countries to improve hydrocephalus care and start their own research efforts.
- Children we treat have the option to take part in clinical trials of promising new treatments. They can be especially important if your child’s condition is not well controlled with standard medicines or surgeries.
Read about Seattle Children’s hydrocephalus research.
-
Specialists in caring for kids and teens
- Children don’t react to illness, pain, medicine or surgery in the same way as adults. They need – and deserve –care designed just for them. They need a healthcare team specially trained to understand and meet their needs. We are that team.
- Our doctors have special training in how to diagnose and treat children. They are focused on how today’s treatment will affect your child as they develop and become an adult.
- Our experts base their treatment plans on years of experience and the newest research on what works best – and most safely – for children and teens.
-
Support for your whole family
- Having a child with hydrocephalus can be stressful for the whole family. For children who need urgent treatment, Seattle Children’s is the only hospital in the region with coverage 24 hours a day, 7 days a week by a pediatric neurosurgeon. Our Emergency Department offers round-the-clock access to Seattle Children’s specialists and the full facilities of our hospital.
- During visits, we take time to explain your child’s condition. We help you fully understand your treatment options and make the choices that are right for your family.
- Our doctors, nurses, child life specialists and social workers help your child and your family through the challenges of their condition. We connect you to community resources and support groups.
- At Seattle Children’s, we work with many children and families from around the Northwest and beyond. We can help with financial counseling, schooling, housing, transportation, interpreter services and spiritual care. Read about our services for patients and families.
Symptoms of Hydrocephalus
Symptoms are different in babies and in older children.
-
Symptoms in babies
In babies, the most common symptoms are:
- Head growth that is larger than normal.
- Bulging “soft spots” (fontanelles) on your baby’s head that may be soft or firm.
- Wide spots between the flat bones of the skull (splayed sutures).
- Eyes that seem to look down all the time (sunsetting eyes). The white part of the eye can be seen above the colored part. The colored part is partly covered by the lower eyelid. This gives your baby a surprised look.
- Developmental delays.
- Poor eating.
- High-pitched cry.
- Sleepiness.
- Crankiness.
-
Childhood symptoms
Children who develop hydrocephalus often have these symptoms:
- Headache
- Nausea and vomiting
- Low energy and sleepiness
- Less ability to understand
- Memory problems
- Vision changes
Diagnosing Hydrocephalus
Doctors will examine your child, looking for signs of hydrocephalus. Doctors also use imaging studies to see signs of hydrocephalus. These tests include:
- Ultrasound
- CT (computed tomography) scan
- MRI (magnetic resonance imaging)
- 3-D imaging, a very accurate way to measure fluid in the brain
At Seattle Children’s we also use methods such as low-dose CT scans and rapid-sequence MRI that lower your child’s exposure to radiation.
Treating Hydrocephalus
Most children with hydrocephalus need surgery to help CSF drain from their head. For some children, it also helps to heat part of the brain so it makes less CSF. Normally, your child’s body makes about a pint of CSF each day.
Treatment options include:
- Using a tube (shunt) to drain CSF to another part of the body where it is absorbed
- Making a channel in the brain so CSF can flow a different way (endoscopic third ventriculostomy or ETV)
- Heating part of the ventricles in the brain so the tissue makes less CSF (choroid plexus cauterization or CPC)
Sometimes neurosurgeons treat hydrocephalus with an endoscope, a thin tube that carries a light and a camera. This tool lets surgeons see inside the body and perform surgeries. Using an endoscope (endoscopy) lets surgeons make smaller cuts (incisions) than open surgery. This is called minimally invasive.
-
Surgery to place a shunt
The most common treatment for hydrocephalus is surgery to put in a tube (shunt). The shunt drains extra CSF from ventricles in your child’s brain to another part of their body. There, the fluid is absorbed. Draining extra CSF from the brain creates normal pressure inside your child’s head.
The tube may drain CSF into:
- The belly (abdomen). This is most common. It is called a ventriculoperitoneal (ven-trick-yoo-lo-pair-ih-tuh-NEE-ahl) shunt or a VP shunt.
- An upper chamber in the heart (atrium).
- The lining of the lung.
The shunt has 3 parts:
- A tube that goes into 1 of the brain ventricles where fluid is building up.
- A valve that makes fluid flow away from the brain (not into it). The valve also controls how much fluid drains out. This controls the pressure in your child’s head.
- A tube that comes off the valve and goes into another part of the body.
We place shunts with “GPS guidance,” using stereotactic computer-assisted navigation during surgery.
Our neurosurgeons use different shunts and valves, based on your child’s needs. One type of valve can be adjusted from the outside by a small magnet. Any time your child has MRI (magnetic resonance imaging), this type of valve must be reset. Our neurosurgery nurse practitioners can reset these valves.
-
Endoscopic treatment of multiloculated hydrocephalus
Surgeons use an endoscope to treat a complex condition called multiloculated hydrocephalus. This condition happens when bleeding or infection causes scars within the ventricles of the brain. The scarring creates many small pockets of CSF that do not connect with each other.
In the past, doctors placed a separate shunt in each pocket that held fluid. Now, using an endoscope, they can make small holes in the pockets. This connects the pockets so your child needs only 1 shunt.
-
Endoscopic third ventriculostomy (ETV)
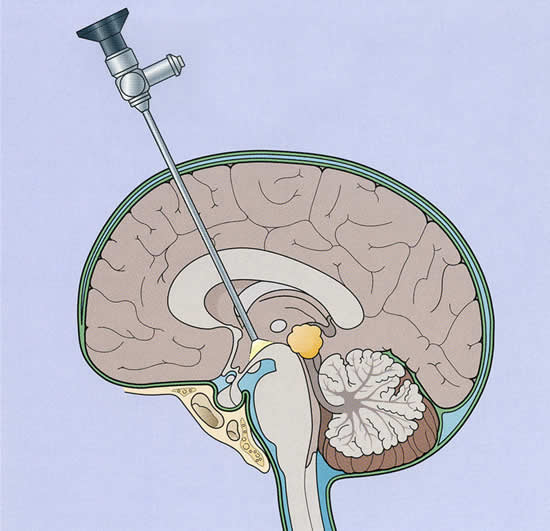
An endoscope being used to make a hole in the ventricle so the patient can avoid needing a shunt.
For a small number of children, an endoscopic third ventriculostomy (ETV) surgery may be a treatment option. This surgery replaces the need for a shunt. Most often it’s done in children who have a narrow or blocked channel leading out of their ventricles (aqueductal stenosis). Depending on your child’s brain structures and age, the neurosurgeon may talk with you about doing an ETV instead of putting in a shunt.
During an ETV, the neurosurgeon:
- Makes a small hole in your child’s skull
- Uses a rigid endoscope to go into the third ventricle and make a hole in the bottom of it
CSF flows out of this hole and reaches the normal places around the brain where it is absorbed.
Children who have an ETV may avoid complications that can happen with shunts, such as infections or needing a shunt replaced (shunt revision). In carefully selected patients, ETV has a high success rate. But some children who have an ETV need to have a shunt put in later.
-
Choroid plexus cauterization (CPC)
If your child’s body is not absorbing CSF well, a choroid plexus cauterization (CPC) may be a treatment option. This procedure lowers the amount of CSF your child’s brain makes. It is done during the same surgery as ETV.
In CPC, the neurosurgeon:
- Uses a flexible endoscope to reach the choroid plexus in the lateral ventricles in each side of the brain
- Sends an electric current to this tissue
The current burns the tissue so it doesn’t make as much CSF. With less CSF produced, fluid may no longer build up. This may avoid the need for a shunt in the future.
Contact Us
If you would like an appointment, ask your child’s primary care provider for a referral. If you have a referral, call 206-987-2016 to make an appointment.
Providers, see how to refer a patient.
If you have questions, contact us at 206-987-2016 or 844-935-3467 (toll-free).
-
Schedule an appointment with the Neurosciences Center
If this is a medical emergency, call 911.
- If you would like an appointment, ask your child’s primary care provider for a referral.
- If you have a referral, call 206-987-2016 or 844-935-3467 (toll-free).
- How to schedule.
If you have any questions, please contact us at 206-987-2016 or 844-935-3467 (toll-free).
-
Find a doctor
- Meet the Neurosciences team.
-
Locations
- Seattle Children’s hospital campus: 206-987-2016 or 844-935-3467 (toll-free)
- Bellevue Clinic and Surgery Center: 206-987-2016 or 844-935-3467 (toll-free)
- Everett: 425-783-6200
- Federal Way: 206-987-2016 or 844-935-3467 (toll-free)
- Olympia: 206-987-2016 or 844-935-3467 (toll-free)
- Tri-Cities: 206-987-2016 or 844-935-3467 (toll-free)
- Wenatchee: 206-987-2016 or 844-935-3467 (toll-free)
-
Refer a patient
- Urgent consultations (providers only): call 206-987-7777 or 877-985-4637 (toll free).
- If you are a provider, fax a New Appointment Request Form (NARF) (PDF) (DOC) to 206-985-3121 or 866-985-3121 (toll-free).
- Send the NARF, chart notes and any relevant documentation to 206-985-3121 or 866-985-3121 (toll-free).