Hyperlordosis
-
Schedule an appointment with Orthopedics and Sports Medicine
- For appointments, call 206-987-2109.
- How to schedule
- Need a second opinion? Call 206-987-2109.
If this is a medical emergency, call 911.
-
Find a doctor
-
Locations
-
Refer a patient
- View our hip dysplasia algorithm to help triage and answer questions about when to refer a patient for hip dysplasia.
- Due to the high volume of infant hip dysplasia referrals, we ask that patients with normal (stable) hip exams be screened following the AAP guidelines
- Urgent consultations (providers only): call 206-987-7777or, toll-free, 877-985-4637.
- If you are a provider, fax a New Appointment Request Form (NARF) (PDF) (DOC) to 206-985-3121 or 866-985-3121 (toll-free).
- View our complete Orthopedics Referral Information.
What is lordosis?
Lordosis (lor-DOE-sis) is the normal shape of the spine in the lower back and neck. In these two areas, a normal spine has a mild backward curve.
Doctors use the term hyperlordosis to refer to curves that are greater than the usual range. You may also hear doctors call this simply “lordosis.”
-
Who gets hyperlordosis?
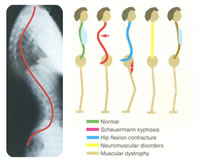
Patterns of sagittal deformity.
Hyperlordosis is rare in children. We usually see it only in those who have nervous system and muscle problems (neuromuscular conditions). These conditions include:
- Cerebral palsy
- Myelomeningocele
- Muscular Dystrophy (MD)
- Spinal muscular atrophy
- Arthrogryposis
Hyperlordosis often happens because muscles near the hips are weak or tightened up. This causes the child’s pelvis to tilt forward and lordosis in the lower part of the spine to increase.
Hyperlordosis at Seattle Children’s
The Spine Program at Seattle Children’s brings together a team of specialists to treat hyperlordosis in babies, children, teens and young adults using nonsurgical and surgical methods.
We treat hundreds of children with neuromuscular spine problems such as hyperlordosis, and our team is known nationally for treating all kinds of spinal deformities in children.
-
The experts you need are here
- The Spine Program team includes doctors, surgeons, physician assistants and nurse practitioners from Orthopedics and Sports Medicine, developmental pediatrics and Rehabilitation Medicine.
- We offer your child the support of an entire medical center. Based on your child’s needs, we involve specialists from other areas of Seattle Children’s.
- Nonsurgical treatment commonly means physical therapy or an aid, like a walker, to help your child stand upright. We have the largest team of physical therapists in the Pacific Northwest who specialize in the care of babies, children, teens and young adults.
- If your child needs surgery, our pediatric orthopedic surgeons have expanded fellowship training in spine problems.
-
Care from birth through young adulthood
- Babies, children and teens are still developing. When we evaluate your child’s hyperlordosis, design their treatment and provide their care, we carefully consider how growth may affect your child’s spinal curve over time – and how their spinal curve may affect the rest of their development and health.
- Our experts are skilled in treating the youngest patients through young adults.
- We have the largest group of board-certified pediatric radiologists in the Northwest. If your child needs imaging that uses radiation, we use the lowest amount possible (PDF) to produce the best image.
-
Our approach to surgery improves quality of life
- Before recommending any surgery, we look at your child as a whole person and take into account many factors, including the degree of their spinal curve, the effects on their health, their remaining growth and what results you can expect from treatment.
- Our surgical spinal cord monitoring team leads the country in developing new techniques for making back surgery safer. We have developed recent advances in spinal cord monitoring and treatment of scoliosis in very young children. Neuromonitoring helps us prevent a spinal cord injury during surgery.
- We have the technology and expertise to precisely place hardware, such as rods and screws, in your child’s spine, including with CT (computed tomography)–guided surgery.
-
Support for your whole family
- Your child’s team works together not only to plan and provide care for your child, but also to make sure you and your child understand your child’s condition and treatment options.
- Coordination is easier for you because your team members from the Spine Program work closely with each other and with other specialized programs and clinics your child may need, like the Neuromuscular Clinic for muscular dystrophy or the Ortho Rehab Clinic for cerebral palsy.
- Seattle Children’s supports your family with a range of resources, such as Child Life specialists, the Family Resource Center and Guest Services.
Symptoms of Hyperlordosis
The main sign of hyperlordosis is a swayback look in both children and adults. Hyperlordosis can make their bottoms stand out.
Diagnosing Hyperlordosis
When your child comes to our clinic, we take an X-ray of the spine to see how much it curves. We will look for any problems with the nervous system or muscles that might be related to hype-lordosis. We also will check your child’s hips since hyperlordosis is sometimes is a sign of hip dislocation.
Treating Hyperlordosis
At Seattle Children’s, we use both nonsurgical treatments and surgery to treat hyperlordosis. Most children with hyperlordosis do not need surgery.
-
Mobility aids and physical therapy
Children who have hyperlordosis may need help to get around. When fitted properly, walkers or crutches can help children with disabilities stand more upright.
Physical therapy programs also can often help children with hyperlordosis.
Treating Knee and Kneecap Problems
We tailor treatment to help your child’s specific problem. For most cases of kneecap pain, we emphasize PT, including sports PT, and home exercise programs.
Seattle Children’s has physical therapists and facilities especially for children and teens. If your child needs surgery, we have pediatric orthopedic surgeons with the training and experience to repair children’s knee problems.
-
Physical therapy and exercise
Physical therapy and home exercise programs strengthen muscles around the knee so that the kneecap stays in place.
Exercises to strengthen the muscle on the inside of the front of the thigh (medial quadriceps) are especially important to treating kneecap problems successfully. When this muscle is strong, it helps keep the kneecap tracking correctly.
-
Surgery for hyperlordosis
If your child needs surgery to correct their curve and stabilize their spine, doctors usually operate on both the front and the back of the spine. This helps them better correct the deformity.
In this surgery, the doctor will:
- Put hooks or screws in the bones of the back (vertebrae).
- Remove the joints between the bones.
- Attach a metal rod to the hooks or screws.
- Reposition your child’s spine to be straighter.
- Tighten the screws or hooks to make sure they are firmly attached to the rod.
- Place a bone graft along the spine to help the vertebrae grow together.
These operations are often complex, so most of our patients stay in our Pediatric Intensive Care Unit after surgery.
Contact Us
Contact Orthopedics and Sports Medicine at 206-987-2109 for an appointment, a second opinion or more information.
Providers, see how to refer a patient.
-
Schedule an appointment with Orthopedics and Sports Medicine
- For appointments, call 206-987-2109.
- How to schedule
- Need a second opinion? Call 206-987-2109.
If this is a medical emergency, call 911.
-
Find a doctor
-
Locations
-
Refer a patient
- View our hip dysplasia algorithm to help triage and answer questions about when to refer a patient for hip dysplasia.
- Due to the high volume of infant hip dysplasia referrals, we ask that patients with normal (stable) hip exams be screened following the AAP guidelines
- Urgent consultations (providers only): call 206-987-7777or, toll-free, 877-985-4637.
- If you are a provider, fax a New Appointment Request Form (NARF) (PDF) (DOC) to 206-985-3121 or 866-985-3121 (toll-free).
- View our complete Orthopedics Referral Information.