Tracheoesophageal Fistula and Esophageal Atresia
-
Schedule an appointment with the Tracheoesophageal Fistula and Esophageal Atresia Program
- Talk with your pregnancy care provider if TEF/EA is suspected before birth. If your child has a history of TEF/EA, contact your pediatrician or primary care provider
- If you have a referral, call 206-987-5963 to schedule an appointment.
- How to schedule
If this is a medical emergency, call 911.
-
Find a doctor
- Meet the Airway and Esophageal Center team.
-
Locations
- Airway and Esophageal Center at Seattle Children's Hospital Campus
-
Refer a patient
- Providers, read how to refer patients.
What is Tracheoesophageal Fistula and Esophageal Atresia?
Tracheoesophageal Fistula (TEF) and Esophageal Atresia (EA) happen while a baby is growing during pregnancy. Most often, TEF and EA happen together. But sometimes a child has 1 condition and not the other. Each name refers to a specific problem.
Doctors are not sure what causes these rare problems. They are present when a child is born (congenital). TEF and EA are not thought to be passed from parent to child (inherited).
Tracheoesophageal fistula:
The word fistula (FIS-chu-luh) means “abnormal connection.” Tracheoesophageal (TRAY-kee-oh-ee-SAH-fuh-JEE-ul) fistula happens when a baby’s windpipe (trachea) and food tube (esophagus) are connected. Food and saliva can get into the trachea and lungs through this channel. This can make a child cough or choke and lead to lung infections such as pneumonia.
Esophageal atresia:
Esophageal atresia (ee-SAH-fuh-JEE-ul uh-TREE-zhuh) happens when the tube that leads from the mouth to the stomach (esophagus) does not form before birth. The tube leading down from the mouth and the tube leading up from the stomach do not meet. A baby with EA cannot feed by mouth, because there is no way for food and liquid to travel from their mouth to their stomach.
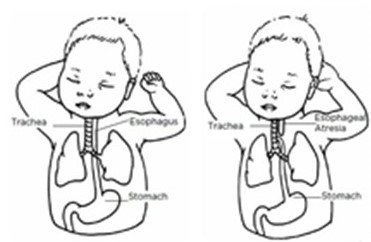
(Left illustration) Normal anatomy. (Right illustration) Esophageal atresia (EA) with distal tracheoesophageal fistula (TEF).
What are the most common types of TEF/EA?
TEF/EA can take several forms. The most common form (pictured on the left) is when the upper part of the food tube (esophagus) has a closed end and the lower part connects to the windpipe (trachea). It is called esophageal atresia with distal tracheoesophageal fistula.
Other medical conditions linked to TEF/EA:
Some babies have other conditions that are linked to TEF and EA. The problems may affect a baby’s heart, kidneys, digestive tract or bones. Doctors call this the VACTERL association.
Each letter stands for a possible different condition:
- V = vertebral, concerns with the bones in the spine
- A = imperforate anus, when the baby's anus or rectum does not form properly
- C = cardiac, complications with the heart
- TE = tracheoesophageal fistula and esophageal atresia
- R = renal (kidney) problems
- L = limb, challenges with bones in the arms or legs
TEF/EA at Seattle Children’s Hospital
Seattle Children’s has the only team in the region with expertise in all the areas that babies and children with TEF/EA may need. Sometimes care starts before birth if an ultrasound during pregnancy suggests your baby has TEF/EA.
If you would like an appointment, ask your primary care provider to refer you to our Tracheoesophageal Fistula and Esophageal Atresia Program. If you would like more information or have a referral, call 206-987-5963 or fax to 206-985- 3392 to make an appointment. Providers, see how to refer a patient.
What are the symptoms of TEF and EA?
- Symptoms of TEF/EA: Breathing problems and coughing or choking when your baby tries to swallow. The symptoms show up right after birth. This requires immediate attention with a specialty team.
- Symptoms of TEF only: Severe coughing or choking when your baby tries to swallow, usually after feeding. Some babies may have trouble breathing while feeding. If your baby has TEF alone, it may be weeks or months after birth before TEF is diagnosed as the cause of symptoms.
- Symptoms of EA only: Your baby is not swallowing their saliva, is drooling a lot or has foamy mucus in their mouth or nose. Most often, EA alone is diagnosed before birth or right after birth. This requires immediate attention with a pediatric specialty team.
How are tracheoesophageal fistula and esophageal atresia diagnosed?
Ultrasound
Sometimes doctors can diagnose TEF/EA before your baby is born based on the results of a prenatal ultrasound. Our Fetal Care and Treatment Center can help your family and your obstetricians get ready for the birth and plan your baby’s care.
Nasogastric tube and X-ray
If doctors suspect your newborn has TEF/EA, they try to pass a tube from your baby’s nose or mouth into their stomach. The tube is called a nasogastric tube or NG tube.
If a baby has EA, the NG tube hits a blocked end, often in the mid-chest. Doctors can see this blockage on an X-ray. Often that is the only diagnostic test needed. Your baby would be moved from their birth hospital to Seattle Children’s right away.
Babies who have only EA do not show gas in their stomachs. Because the esophagus has not formed properly in EA, the only way gas can get into the stomach is through an abnormal connection between the windpipe and the esophagus. If a child also has TEF, an X-ray will show gas in the baby’s stomach.
Contrast studies
To find TEF without EA, doctors sometimes use a test called an esophagram. First, your child swallows a liquid (gastrograffin or barium). The liquid helps to fill the spaces in the tube from the mouth to the stomach (esophagus). If there is a TEF, the liquid will be seen traveling from the esophagus into the windpipe via a connection of tissue. It will show on the X-ray screen.
The doctor may take a series of X-rays to look at the esophagus, stomach and the first part of the small bowel. First, we give your child a contrast liquid that shows up on X-ray. This test is called an upper GI (gastrointestinal) series (PDF) (Spanish).
Test to find related problems
We will check all babies with TEF/EA for other possible related problems. These tests include:
- X-rays and ultrasound to check for problems with bones in the spine, arms or legs
- Ultrasound of their heart (echocardiogram or echo)
- Ultrasound and possibly other tests of their kidneys
- Exam to see how well the anus is formed
If your baby has any of these problems, the doctor will explain other tests or treatment they need.
Treating Tracheoesophageal Fistula and Esophageal Atresia
Babies with EA, with or without TEF, will need surgery soon after they are born. The type of surgery depends on your baby’s condition. In many cases, surgeons correct the problem with 1 surgery. Other times, doctors need to correct it in stages. Your baby’s surgeon will talk with you about the best option for your child.
-
Care soon after birth
Our transport team is very experienced in safely moving fragile babies to Seattle Children’s from their birth hospital. In our Level 4 Neonatal Intensive Care Unit (NICU), we will give your baby the highest level of care.
We carefully assess your child to decide the best treatment for them. This includes any breathing support they need and the timing of surgery.
About one-third of children born with TEF, EA or TEF/EA are born early. This may happen because babies with EA cannot swallow normal amounts of amniotic fluid and it builds up inside the mother’s womb. Premature babies may need breathing support and treatment for other health problems at birth.
Before surgery, your baby’s doctors will:
- Stabilize your baby’s health.
- Give your baby fluids through an IV (intravenous) line into their vein.
- Place a tube through your baby’s nose into their esophageal pouch. The tube helps keep air and fluid out of the pouch so your baby is less likely to breathe spit (saliva) into their lungs.
- Do an ultrasound of the heart (echocardiogram). This helps ensure the surgery can be done as safely as possible.
- Give your child medicine to make them sleep without pain during the surgery (general anesthesia). Our doctors are board certified in pediatric anesthesiology, with extra years of training in how to give pain medicine to babies and children safely.
-
Surgery for TEF and EA combined
The surgeon will:
- Make a cut (incision) in your child’s chest, usually on the right side
- Find the abnormal channel (fistula) between the windpipe and esophagus
- Cut through the channel and sew it closed
If the ends of the esophagus are close enough to each other, the surgeon will join them with stitches.
If the ends of the esophagus are too far apart to connect safely, the surgeon will not repair the esophagus. The surgeon will:
- Place a feeding tube in your child’s stomach. This is called a gastrostomy (gas-STRAH-stuh-mee) tube.
- Repair your baby’s esophagus through aa series of procedures over time.
- Talk with you about the options.
-
Surgery for TEF only
If your baby has TEF but not EA, doctors most often repair it through a small cut in your baby’s neck. The surgeon will:
- Find the fistula
- Cut through it
- Sew the trachea and esophagus closed
-
Surgery for EA only
If your baby has EA but not TEF, the 2 ends of the esophagus are too far apart to sew together right away. In this case, your baby will need surgery to place a feeding tube through their belly wall. This is called a gastrostomy. It is how your baby will get nutrition until they have surgery to fix their esophagus.
Doctors will wait until your baby grows larger before doing the surgery to sew the esophagus together. This gives the esophagus time to grow so the 2 ends may get closer together.
Sometimes, the 2 ends stay far apart. There are different ways to repair or even replace the esophagus. Your surgeon will talk with you about these options.
-
Gastrostomy
A gastrostomy is a safe way to give your baby nutrition until they can feed by mouth. The surgeon:
- Makes an opening through the wall of your baby’s belly
- Places a G (gastromy) tube into their stomach
Your baby receives nutrients through this tube, and medicine if needed.
We will teach you how to take care of the tube and how to feed your child through it.
Your surgeon will take out the G tube after your baby can eat by mouth. Some babies will need the G tube for several months or even longer. This is because they need to learn to swallow after esophagus repair.
-
After surgery
After surgery for TEF/EA or EA, your baby will likely need a machine to help them breathe (ventilator). It may be a few days to a week or more before your baby can breathe well on their own. If your baby had surgery for TEF alone, they will only need a breathing machine during surgery.
After surgery, we will give your child:
- Pain medicine for their comfort
- Fluids and nutrition through an IV (intravenous) tube into a vein
-
Nutrition and feeding
About a week after your baby’s surgery, we will do an imaging study to check the esophagus repair for leaks. This is called an esophagram. If there is no leak, your baby may be able to start feeding by mouth.
Most babies start feeding slowly. Your baby may not be able to get all their nutrition by mouth for several days or weeks. Some babies need extra feedings from a tube passed through their nose and into their stomach. This is called a NC (nasogastric) tube. Babies who had a gastrostomy tube placed early in life will keep using that until they can take all their feedings by mouth.
How long your child will need some or all of their nutrition by tube depends on:
- How well they swallow.
- If they have problems with stomach contents flowing backwards into the esophagus (gastroesophageal reflux or GER). With a feeding tube, your baby can still feed by mouth if they are able. As needed, they can get breast milk or formula through the feeding tube.
Our nurses and lactation specialists will do all that we can to support you in giving your baby breast milk. To keep your milk flowing and to build a milk supply for your baby, we help you with breast pumping and storing your milk. When your baby is ready, our nurses and feeding therapists help with the transition to feeding by bottle or breast.
Our nutritionists keep a careful watch on your baby to be sure they are growing well. Our feeding therapists help your child learn to feed by mouth.
-
How long will my child be in the hospital?
The hospital stay for babies with TEF and EA varies. If your baby is healthy and the repair is simple, they will likely stay for 2 weeks or a little longer.
Your baby may need to stay in the hospital for many more weeks if:
- They have other health problems
- They have EA but not TEF
- Doctors have to wait to do surgery
Your baby will be ready to go home when they are breathing well and have a feeding plan to help them gain weight.
Before your baby goes home, we will teach you:
- How to care for the incisions
- About medicine they need
- How to feed your child using a tube in their nose (NG tube) or stomach (G tube)
- Signs of problems to watch for
Our nurses will help set up any supplies and equipment you need. You will have plenty of time to practice all your baby’s care before going home.
-
Ongoing care to young adulthood
About 1 to 3 weeks after your baby leaves the hospital, they will see the surgeon for a follow-up visit to make sure:
- Your baby is breathing well
- Their incision is healing
- Your child is feeding, gaining weight and growing well
- There are no other health problems
Our Tracheoesophageal Fistula and Esophageal Atresia Program team, including specialists in pulmonology, gastroenterology, otolaryngology, nutrition and feeding, will give your child the follow-up care they need.
- We help with any feeding problems. As children with TEF/EA grow, they may have difficulty swallowing liquids without it getting into their airway. They may need to eat more slowly and chew more than other people. Speech language pathologists can recommend specific treatments based on your child’s age and feeding abilities.
- The most common long-term problem for babies with TEF/EA is stomach contents flowing backwards into the esophagus (gastroesophageal reflux or GER). This can be related to the structural shape of the esophagus. Foods your child eats can also cause reflux. The esophagus may be more sensitive and allergic to specific food groups. We often can treat this with medicine.
- We may need ongoing diagnostic pictures like esophagrams and a visual scope into the esophagus. If your child’s reflux or difficulty eating and swallowing gets worse, your doctor will suggest treatment. They may need to stretch (dilate) the esophagus where the scar formed from their earlier surgeries.
- Children with TEF/EA might have a floppy airway. This can lead to more symptoms like coughing or trouble breathing. They may get more colds or other respiratory illnesses that seem to last longer or are more intense. Preventing illness is incredibly important and requires routine involvement with the lung doctor (pulmonologist) with the TEF/EA team.
Our team of experts will work with you to check your child’s health until they reach early adulthood. We provide ongoing support and resources for you and your child.
Contact Us
For more information, call the Tracheoesophageal Fistula and Esophageal Atresia Program at 206-987-5963. If you would like an appointment, ask your child’s primary care provider for a referral
[NB1]Internet phone link.
Providers: See how to refer a patient.
-
Schedule an appointment with the Tracheoesophageal Fistula and Esophageal Atresia Program
- Talk with your pregnancy care provider if TEF/EA is suspected before birth. If your child has a history of TEF/EA, contact your pediatrician or primary care provider
- If you have a referral, call 206-987-5963 to schedule an appointment.
- How to schedule
If this is a medical emergency, call 911.
-
Find a doctor
- Meet the Airway and Esophageal Center team.
-
Locations
- Airway and Esophageal Center at Seattle Children's Hospital Campus
-
Refer a patient
- Providers, read how to refer patients.
