Current Research
Current Active Projects
The Debley Lab's current active projects include:
Dysregulated asthmatic epithelial interferon responses to viruses drive exacerbation, T2 inflammation, and airway remodeling – NIH/NIAID R01AI163160 (Debley – Principal Investigator)
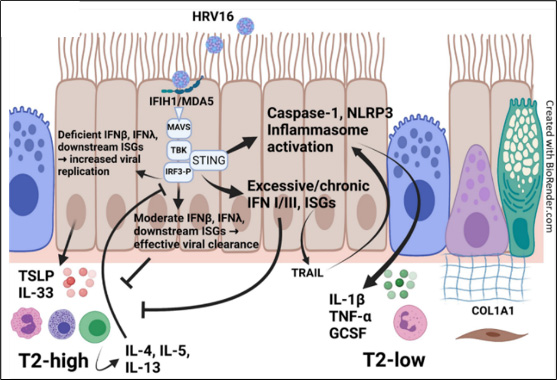 In our cohort of well characterized asthmatic children, from whom we obtain bronchial AECs and conduct mechanistic ex vivo experiments using organotypic models, we have observed marked heterogeneity in IFN I/III responses to HRV and RSV infection, with greater HRV replication in AECs from exacerbation-prone asthmatics. We recently observed greater production of the T2 alarmins TSLP and IL-33 by asthmatic AECs with the lowest IFNλ responses to HRV, while AECs with the greatest IFNλ responses also had the greatest production of T2-low/NLRP3 inflammasome-associated cytokines IL-1β and TNF-α. These observations, inform our global hypotheses that the magnitude and kinetics of AEC IFN responses to HRV influence T2-high and T2-low asthma endotypes, with moderate self-limited IFN responses essential to limit viral replication, reduce exacerbation risk, and dampen T2 inflammation, while exaggerated IFN responses enhance the NLRP3 inflammasome and production of T2-low cytokines (IL-1β, TNF-α), neutrophilic and inflammation, airway remodeling, and lung function decline. Furthermore, we hypothesize that a common polymorphism in the viral sensor IFIH1/MDA5 (rs1990760), recently associated with asthma, contributes to dysregulated AEC IFN responses to HRV. Finally, we will use a humanized mouse expressing hICAM1 to allow HRV-A infection, in the context of differential MDA5 function, to test in vivo the role of these pathways in HRV-A infection, T2-high vs. T2-low airway inflammation, exacerbation, and airway remodeling.
In our cohort of well characterized asthmatic children, from whom we obtain bronchial AECs and conduct mechanistic ex vivo experiments using organotypic models, we have observed marked heterogeneity in IFN I/III responses to HRV and RSV infection, with greater HRV replication in AECs from exacerbation-prone asthmatics. We recently observed greater production of the T2 alarmins TSLP and IL-33 by asthmatic AECs with the lowest IFNλ responses to HRV, while AECs with the greatest IFNλ responses also had the greatest production of T2-low/NLRP3 inflammasome-associated cytokines IL-1β and TNF-α. These observations, inform our global hypotheses that the magnitude and kinetics of AEC IFN responses to HRV influence T2-high and T2-low asthma endotypes, with moderate self-limited IFN responses essential to limit viral replication, reduce exacerbation risk, and dampen T2 inflammation, while exaggerated IFN responses enhance the NLRP3 inflammasome and production of T2-low cytokines (IL-1β, TNF-α), neutrophilic and inflammation, airway remodeling, and lung function decline. Furthermore, we hypothesize that a common polymorphism in the viral sensor IFIH1/MDA5 (rs1990760), recently associated with asthma, contributes to dysregulated AEC IFN responses to HRV. Finally, we will use a humanized mouse expressing hICAM1 to allow HRV-A infection, in the context of differential MDA5 function, to test in vivo the role of these pathways in HRV-A infection, T2-high vs. T2-low airway inflammation, exacerbation, and airway remodeling.
Seattle AADCRC U19 – Epithelial Immune Responses During Respiratory Viral Exacerbation of Asthma – NIH/NIAID U19AI175089 (Debley – Co-Principal Investigator)
Lower respiratory tract viral infections serve as the dominant trigger for the onset and progression of asthma. Although asthma management has shifted towards targeting airway inflammation at all levels of the disease, primarily with inhaled corticosteroids (ICS) and biologic therapies targeting type-2 (T2) inflammation, there is a substantial burden of disease that is not responsive to these therapies. Specifically, a substantial portion of individuals treated with ICS therapy have persistent T2 inflammation in their lower airways and a large and growing portion of individuals with asthma have inflammation of the airways that is not T2 predominant (non- T2). These related phenomena of persistent T2 (T2-high) and non-T2 inflammation in asthma are emerging as the most common phenotypes in adults, and now make up a substantial portion of children with the disease. The mechanisms responsible for persistent T2 and non-T2 inflammation are incompletely understood, but there is strong evidence that the epithelium and epithelial-derived cytokines play a major role in the immunology of asthma, and we have recently demonstrated that the epithelium is infiltrated with specific innate immune cells that interact with the epithelium to propagate and regulate inflammation. Our central hypothesis is that the airway epithelium serves as a central coordinator of the immune response to viral respiratory tract infection in asthma. Further, airway epithelial cells (AECs) from T2-high and non-T2 individuals differentially interact with immune cells to support inflammation in a manner that can be identified and targeted. We have an established program to isolate AECs from children and adults to examine the function of these cells in asthma using a combination of organotypic cell culture models, often in combination with immune cells. The primary goals of the Seattle Center are to identify primary alterations in AECs in asthma, understand how AECs differ between T2-high and non-T2 individuals, and characterize interactions between the epithelium and immune cells that are in close proximity. In Project 1, we examine the underpinnings of persistent T2 inflammation mediated through mast cells and eosinophils acting in conjunction with the epithelium and the components of this inflammation that are resistant to corticosteroids. In Project 2, we examine the basis of interactions between the epithelium and macrophages, Th17 cells, and neutrophils and how epithelial cells from each of the groups support inflammation through these cells. These projects are supported by Pediatric and Adult Epithelial Cores (Core B) to isolate AECs from well phenotyped adults and children and further examine connections between phenotype, genomics, genotype, and clinical outcome. The studies are supported by an Advanced Bioinformatics Core (Core C) using state of the art single cell and bulk RNA sequencing. These studies will facilitate the precise targeting of inflammation based on clinical phenotype and epithelial endotype and a greater understanding of the basis of interactions between the epithelium and immune cells that reside within the epithelium in asthma.
Seattle AADCRC U19 – Human Airway Epithelial Cell Culture Core – NIH/NIAID U19AI175089 (Debley – Project Leader)
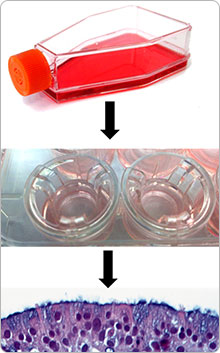 The primary goal of Core B Airway Epithelial Cell Culture Core is to support the Seattle Center projects by providing organotypic cultures of epithelial cells from carefully phenotyped individuals. The core is divided into a pediatric sub-core and an adult sub-core. Core personnel will identify individuals scheduled for elective surgery, explain the study, and obtain informed consent. Epithelial cells are collected from enrolled individuals at the time of elective surgery by bronchial brushing via a secure endotracheal tube. Epithelial cells are expanded in submerged culture and either stored or used immediately as needed for differentiated air-liquid interface organotypic cultures to support the co-culture model systems in the two projects. A key function of the Core is to carefully characterize individuals with asthma into T2-high and non-T2 clinical phenotypes, using pre-defined criteria for children and adults. Both sub-cores will also collect epithelial cells from healthy controls for comparisons. The pediatric sub-core will obtain additional longitudinal clinical data, allowing correlation of specific clinical phenotypes and the associated epithelial endotypes with temporal clinical data. The adult sub- core will also obtain airway cells via induced sputum, to assist in airway cell endotyping via determination of the Type 2 Gene Mean (T2GM) and to provide airway cells for single cell RNA for sequencing. The adult sub- core will also continue to expand a biorepository of adult airway epithelial cells obtained from donor lung bronchial rings, which are discarded at the time of lung transplant. This provides significantly larger numbers of cells per donor as compared to airway brushing. These cells will be provided along with assistance from the core for mechanistic studies, using gene disruption techniques such as shRNA gene silencing or CRISPR/Cas9 gene editing.
The primary goal of Core B Airway Epithelial Cell Culture Core is to support the Seattle Center projects by providing organotypic cultures of epithelial cells from carefully phenotyped individuals. The core is divided into a pediatric sub-core and an adult sub-core. Core personnel will identify individuals scheduled for elective surgery, explain the study, and obtain informed consent. Epithelial cells are collected from enrolled individuals at the time of elective surgery by bronchial brushing via a secure endotracheal tube. Epithelial cells are expanded in submerged culture and either stored or used immediately as needed for differentiated air-liquid interface organotypic cultures to support the co-culture model systems in the two projects. A key function of the Core is to carefully characterize individuals with asthma into T2-high and non-T2 clinical phenotypes, using pre-defined criteria for children and adults. Both sub-cores will also collect epithelial cells from healthy controls for comparisons. The pediatric sub-core will obtain additional longitudinal clinical data, allowing correlation of specific clinical phenotypes and the associated epithelial endotypes with temporal clinical data. The adult sub- core will also obtain airway cells via induced sputum, to assist in airway cell endotyping via determination of the Type 2 Gene Mean (T2GM) and to provide airway cells for single cell RNA for sequencing. The adult sub- core will also continue to expand a biorepository of adult airway epithelial cells obtained from donor lung bronchial rings, which are discarded at the time of lung transplant. This provides significantly larger numbers of cells per donor as compared to airway brushing. These cells will be provided along with assistance from the core for mechanistic studies, using gene disruption techniques such as shRNA gene silencing or CRISPR/Cas9 gene editing.
Seattle AADCRC U19 – Project 2: Epithelial activation of airway inflammation in patients with non-T2 asthma – NIH/NIAID U19AI175089 (Debley – Project Leader)
Therapies for asthma that target type-2 (T2) inflammation are ineffective in many patients with asthma in part due to the increasing number of individuals with non-T2 asthma who have a suboptimal response to standard therapy with inhaled corticosteroids or biologics targeting T2 cytokines. Millions of viral-triggered asthma exacerbations occur annually in this group of patients in the U.S. leading to significant morbidity and cost to the health care system, due in part to the lack of effective treatments for non-T2 asthma for children and adults. The clinical features and airway inflammatory cell infiltrate patterns of non-T2 asthma have been characterized in detail, but the specific role of the airway epithelium in coordinating immune cell responses and influencing exacerbations, lung function, and persistent inflammation in donors with non-T2 asthma remains poorly characterized. Our preliminary studies demonstrate that airway epithelial cells (AECs) from non-T2 asthmatic children exhibit more robust type I and III interferon (IFN) responses and greater “non-T2 cytokine” (IL-1β, TNF-α, IL-17C, and GCSF) production following RV infection as compared to AECs from T2-high donors. In Project 2, we will use bronchial AECs from well characterized cohorts of children and adults with and without asthma to conduct mechanistic ex vivo experiments using organotypic models, to test our central hypothesis that in non-T2 asthma RV infection triggers excessive epithelial production of non-T2 cytokines and/or excessive IFN responses that activate the NLRP3 inflammasome, leading to neutrophilic inflammation, airway remodeling, and lung function decline through interactions with Th17 cells and/or lung macrophages. We will extend our ex vivo AEC model to include coculture studies of AECs with both Th17 and lung macrophages, and specifically assess bidirectional interactions utilizing bulk and single cell transcriptomics to assess epithelial-dependent neutrophil activation. We will also utilize cutting edge bioinformatics techniques to assess the genomic and epigenetic alterations in the epithelium that drive non-T2 inflammation as well as relevant in vivo modeling of HRV infection in the setting of non-T2 inflammation.
Clinical Impacts of Heterogeneous Interferon Responses to Viral Infection by Asthmatic Airway Epithelium – NIH/NIAID K24 AI150991 (Debley – Principal Investigator)
Using airway epithelial cells from clinically well characterized asthmatic children, the Debley Lab will investigate the regulation of epithelial interferon responses to viral infection and the impacts of excessive or deficient epithelial interferon responses on incident viral triggered asthma exacerbation risk and lung function over time. The studies conducted in Dr. Debley’s Lab and unique resource of primary airway epithelial cells from clinically well characterized asthmatic children, provide an exceptional training environment for young investigators under Dr. Debley’s mentorship who are dedicated to pursuing a career in mechanistic patient-oriented research to learn translational research techniques to investigate the role of the airway epithelium in pediatric lung diseases and viral infection.
Participate in Research
Help us answer questions about childhood health and illness, and help other children in the future. See our current research studies.