Second Malaria Gene Linked to Drug Resistance
May 24, 2023 – Researchers in the Center for Global Infectious Disease Research (CGIDR) at Seattle Children’s Research Institute and an international team of colleagues have found a second gene is involved in malaria’s resistance to the antimalarial drug chloroquine, upending a long-held belief that only one gene contributes to drug resistance. These findings, published recently in the journal Nature Microbiology, show the complexity of drug resistance and have implications for the ongoing global battle against malaria.
Chloroquine has been used to treat malaria since the 1950s, but due to resistance to the drug, is no longer widely used. Drug resistance emerged first in Southeast Asia and later in Africa. In 2000, researchers identified mutations in the chloroquine resistance transporter gene, pfcrt, that prevented chloroquine from killing parasites. Other antimalarial drugs have since been developed but evolving drug resistance remains a challenge. Currently over 200 million people are infected every year with malaria and tragically, over 600,000 people die from the disease, mostly young children in sub-Saharan Africa.
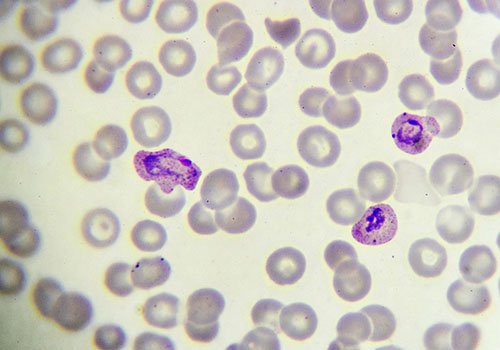
Plasmodium falciparum is the most lethal of the parasites that cause human malaria. For this study, researchers from the Medical Research Council Unit The Gambia at the London School of Hygiene & Tropical Medicine and collaborators analyzed more than 600 P. falciparum genomes collected in The Gambia from 1984 to 2014. The data revealed that mutations in a second gene encoding an amino acid transporter (pfaat1) increased from 0% frequency in 1984 to 97% frequency in 2014, along with mutations in pfcrt.
Teams at Seattle Children’s, Texas Biomed and University of Notre Dame collaborated to evaluate how the mutations in pfaat1 affect drug resistance. Using a combination of genetic crosses and gene editing, researchers demonstrated the role of pfaat1 mutations in chloroquine resistance. Collaborators at Nottingham University tested the gene’s function in yeast, which also showed that the mutations were involved in drug resistance.
“This project would not have been possible without the dedication of multiple collaborators in the U.S., Europe, Asia and Africa,” said one of the paper’s lead authors, Dr. Ashley Vaughan, principal investigator at Seattle Children’s Research Institute and assistant professor of pediatrics at the University of Washington School of Medicine. Vaughan worked closely with CGIDR’s Dr. Stefan Kappe, professor of pediatrics at the University of Washington School of Medicine, and Dr. Sudhir Kumar to show the role of pfaat1 in chloroquine drug resistance.
“We brought together very diverse methodologies, which all came to the same conclusion. This work speaks to the necessity of forming these collaborations to answer the big questions,” Vaughan said. “Research doesn’t happen in a bubble and collaboration is essential to solve the big problems we face in understanding anti-malaria drug resistance.”
Further research suggests that differences in the pfaat1 mutations between global regions may account for the variances in how drug resistance has evolved. “Knowing that more than one gene controls resistance to antimalarial drugs will help us understand drug resistance more fully, aiding in resistance surveillance and the creation of novel interventions,” Vaughan said.
The research team next plans to use further genetic crosses to better understand resistance to the antimalarial drug artemisinin in Africa, which experts fear could halt the progress made to date in preventing death and severe malaria disease there.
Former Vaughan Lab member Meseret Haile also contributed to the research.
The study was supported by numerous grants and sources, including the National Institutes of Health, Medical Research Council, European Research Council, Wellcome Trust, Bill & Melinda Gates Foundation, and the Biotechnology and Biological Sciences Research Council.
— Colleen Steelquist